Великобритания
УДК 781.1 Научные основы. Математические, физические, психологические теории. Музыкальная акустика
Эта статья знакомит читателей со смежными областями звуковой терапии и музыкальной медицины, очерчивая контуры некоторых из многочисленных биологических механизмов, которые были успешно выявлены этими современными направлениями. Для звуковой терапии часто используется общий термин «вибрационная медицина», отражающий энергетическую (вибрационную) взаимосвязь системы разум-тело. Предлагаемая информация предназначена для врачей, психологов, музыкальных терапевтов, медсестер, специалистов интегративной медицины и оздоровительных практик, использующих терапевтический потенциал вибрационной медицины. Поскольку организм использует вибрационную энергию, для поддержки физиологических функций пациента доступен широкий спектр энергетических модальностей. В статье описываются отдельные физиологические механизмы, инициируемые звуковой терапией и музыкальной медициной. Возможно, одним из наиболее важных эффектов является нейтрализация боли, достигаемая с помощью локально применяемых особых звуковых частот. Описаны и другие механизмы, такие как стимуляция блуждающего нерва с помощью прослушивания определенных звуковых частот или музыки через наушники. Статья состоит из двух частей. В первой части представлена краткая история терапии звуком, за которой следуют определения музыкальной терапии, музыкальной медицины и звуковой терапии. Далее описываются некоторые из многих биологических механизмов, активируемых при полном погружении организма в музыку или при воздействиях конкретными звуковыми частотами, включая введение в обезболивание звуком. Часть 2 будет опубликована в следующем номере журнала «Медицина и Искусство». Она описывает прерывание звуком болевого цикла «боль-спазм» при травме позвоночника; облегчение боли и тревожных состояний с помощью точечного массажа и сонопунктуры; кислородное исцеление звуком; музыкальную стимуляцию иммунной системы; звуковую стимуляцию блуждающего нерва через наушники и вокализацию; и наконец, взгляд в будущее вибрационной медицины.
звуковая терапия, музыкальная медицина, вибрационная медицина, ультразвуковые динамики, оксид азота, медиация хронической боли, теория контроля боли
INTRODUCTION
Since the development of quantum physics in the twentieth century, discoveries made in medical physics reveal the body as a complex interplay of biofields [1] in which energy-information flows throughout the organism. At the level of the cell, information is exchanged through electromagnetic signals — primarily in the far infra-red spectrum — in addition to biochemical signals and sonic frequencies [2]. At the atomic level, biological complexities, and energy-information flow, can be viewed in terms of vibration. Nobel Laureate, Max Planck, said:
«As a man who has devoted his whole life to the most clear-headed science, to the study of matter, I can tell you as a result of my research about atoms this much: There is no matter as such. All matter originates only by virtue of a force which brings the particle of an atom to vibration and holds this minute solar system of the atom together» [3].
It is in this context that vibrational medicine has its roots: considering the energetic (vibrational) interconnectedness of the mind-body system. Practitioners of holistic medicine, or functional medicine [4] as it is often referred to, review all aspects of the patient, including their emotions. In this expanded medical model, since the body is comprised of vibrational energy, a wide variety of vibrational and energetic modalities are available to support the patient’s physiology, including sound and music.
Some of the physiological mechanisms initiated by sound therapy and music medicine are achieved by whole-body immersion in specific sound frequencies, or in music, either recorded or live. Other mechanisms, initiated neurologically, can be achieved by listening to specific sounds or music by headphones.
An important yet little discussed aspect of physics, with significant implications for medical science, is that all sounds, whether single frequencies or a complex array of musical frequencies, create far infrared light (FIR), due to the atomic physics of inelastic sonic collisions. The infrared light created by sound and music is why sound intensity is measured in watts per metre squared [5] and such light is modulated in amplitude by the sound, thus, carrying the FIR component of the sonic energy-information almost 4cm into the body’s tissues [6]. As intercellular communication occurs mainly in the far infrared spectrum, the physics of sound-light interactions infers that sonic-modulated light is conveyed to cells in the medium of their own «language» [2].
The author’s studies in acoustic-physics have revealed the quasi-holographic nature of sound in which the identical energy-information is contained throughout the sound ‘wave’, whether emitting from a transducer, a musical instrument or the human voice. However, the actual space-form of audible sound is spherical, therefore, the energy information conveyed by sound and music can be considered to exist at all points on the surface of the sound bubble and within its interior [7].
Audible sounds are quasi-holographic in nature and emit spherically from a sound source.
All points on the bubble’s surface and within its interior, carry identical energy-information (Fig. 1).

Fig. 1. Depiction of a sound bubble emitting from a violin.
(Illustration by Dean Baker)
Рис. 1. Изображение звукового пузыря, исходящего из скрипки. (Иллюстрация Дина Бейкера)
This important fact has far-reaching implications for the future of sound therapy and music medicine, particularly in relation to Faraday Wave patterns that manifest on the surface membranes of cells, organs, visceral fascia and in visceral fluids, a subject we will return to in the last section of this chapter, when we discuss the future of vibrational medicine.
The idea that sounds, in the form of music, can be utilized as a therapy in support of illness is a concept espoused by Pythagoras of Samos, circa 2,500 BCE. One of his biographers, Iamblichus, reported that Pythagoras believed that music could be used in place of medicine and that it contributed greatly to health [8].
Even though his belief is an over-simplification, in fact, sound and music have been shown in recent decades to have many therapeutic effects, as the content of this chapter demonstrates. According to Socrates (436–338 BC), and other writers, Pythagoras of Samos, (circa 570 – circa 495 BC), travelled in Egypt [9,10,11] and absorbed knowledge from their priest-scientists. Music healers practised their craft in ancient Egypt and enjoyed privileged relationships with priests and high-ranking government servants. Music was called ‘physic for the soul’ by Egyptian priest-physicians [12].
The Egyptians built Sanatoria (hospitals) in all major towns. The foundations of the Dendera Sanatorium feature small healing chambers that would have had excellent reverberative qualities, due to their parallel facing walls and flat surfaces, with acoustics similar to modern bathrooms (Fig. 2).

Fig. 2. Dendera Sanatorium (Photo by the author)
Рис. 2. Дендерский санаторий (фото автора)
The Egyptian music healers used conventional musical instruments such as the drum, harp, flute, lyre and tambourine, but ‘sistra,’ were also employed. The sistra is a type of rattle with metal discs that emits significant levels of ultrasound in the 40 to 60 kHz range, which could have supplemented the patients’ beneficial results. Each healing chamber featured a basin containing holy water from the adjacent sacred lake, the water’s miraculous powers were amplified by pouring it over healing statues inscribed with appropriate texts [13]. This principle is not unlike the modern placebo effect, which holds imagined power due to the influence of the patient’s beliefs on their physiology, articulated by Dr. Bruce Lipton in his book, The Biology of Belief [14].
There is also some evidence that the ancient Egyptians employed vowel sound chant (as distinct from singing) for therapeutic effect, just as today humming and chanting are known to stimulate nitric oxide production and to stimulate the vagus nerve, for example, therapies that will be discussed later in the chapter.
The mere sounds of words were considered a potent and creative force in Egypt, as noted by R.A. Schwaller de Lubicz, in his book Sacred Science [15]. Several textual indicators are known regarding the Egyptian’s use of vowel sounds, of which the following are two examples.
A quote from Aristotle, Poetics:
«In Egypt, when priests sing hymns to the gods, they sing the seven vowels in due succession, and the sound of these vowels has such euphony that men listen to it instead of the flute and lyre» [16]. Demetrius, circa 200 BCE.
Such euphony would have been enhanced by vowel sound chant in chambers designed to be reverberative, an acoustic quality that is true of almost all ancient Egyptian temples and tombs.
A letter from Asclepius to King Ammon, from The Corpus Hermeticum:
«The very quality of the sound and pronunciation of the Egyptian language carries itself the power of what is being spoken…We do not use a noise of words [referring to the Greeks] but sounds full of power» [17]. Imhotep (2667-2600 BCE) was the most revered of all physicians in ancient Egypt and was deified by the Egyptians circa 525 BCE. During his lifetime he was vizier to King Djoser and architect of Djoser’s Step Pyramid complex at Saqqara. His legendary abilities include poet, mathematician, astronomer, architect and physician, and in his medical treatise he regarded disease and injury as naturally occurring, not punishments sent by gods [18]. In the Ptolemaic Period, the Greeks identified Imhotep with Asklepios, their god of medicine, and in the second century BCE Ptolemy VIII built a shrine to Imhotep at the great temple of Hatshepsut at Deir el-Bahri, which then became a place of pilgrimage by the sick. The great physician, Sir William Osler pronounced in 1923 that Imhotep was the first figure of a physician to stand out clearly from the mists of antiquity [12].
In the scene from The Feast of Opet, in a building erected by Queen Hatshepsut at Deir el-Bahri, a male harpist and three female musicians perform with sistra instruments (Fig. 3) [19].
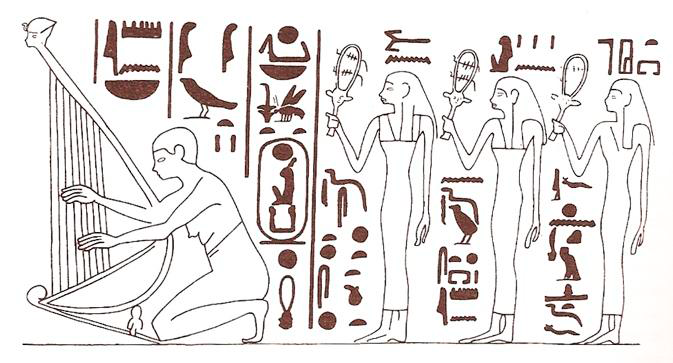
Fig. 3. A scene from The Feast of Opet (A building erected by Queen Hatshepsut at Deir el-Bahri)
Рис. 3. Сцена из «Фестиваля Опета»
(Здание, построенное царицей Хатшепсут в Дейр-эль-Бахри)
Returning to Pythagoras, he proposed that by listening to music one could comprehend and retrace the outer ‘physical’ harmony of the universe, which would lead to a state of inner ‘mental’ harmony, thus re-establishing balance in the body and helping to cure mental disorders [12].
He later founded an intellectual community on the island of Croton, Italy. One group of his followers were known as the «Acoustici», which means «to hear», and from which the word «acoustic» derives.
While Pythagoras is credited with the invention of the monochord — a single gut string tensioned by a fixed weight — which he used for investigating harmonic intervals, the ancient Egyptians had been making and playing musical instruments since pre-dynastic times, a history that had already spanned three millennia by the time of Pythagoras’ visit. Therefore, it seems likely that Pythagoras would have absorbed knowledge of musical intervals, in addition to music as medicine, during his Egyptian travels. Aristotle (384 BCE - 322 BCE), a pupil of Plato, viewed the therapeutic aspect of music as creating an emotional catharsis in mental states and spoke about music imitating passions or states of the soul [12]. An interesting account of music therapy with mental illness comes from Asclepiades of Bythnia (124–40 BCE), the first physician in history to create a health and disease theory resembling what is known today as molecular medicine. Asclepiades was a pioneer in the humane treatment of patients with mental disorders, moving patients out of dark confinements and prescribing work therapy, healthy diet, massages and music therapy [12]. Following Greek culture, no radically new theories and practises of music therapy were reported during a period of roughly 1500 years. However, in the seventeenth and eighteenth centuries there was a flourishing of writings on music and medicine, notably that of the German, Athanasius Kircher (1602-1680) who created an entirely new theory of music’s therapeutic effects. He gave one of the most comprehensive descriptions of music in medicine in his work Phonurgia Nova, in which he laid out the foundation for a therapeutic music style that he called Iatromusic, which is based on acoustic vibrations. The music sets air into vibration, which sets the ‘corpuscles’ of the body into vibration. Kircher proposed a body-mind directed connection: mechanical vibratory energy from the music creates a physical-physiological response in the body, which also brings psychological mind processes into healing harmony [12].
THE ORIGIN OF INAUDIBLE THERAPEUTIC ULTRASOUND AND AUDIBLE SOUND THERAPIES
Therapeutic ultrasound was discovered in 1927 by Professor R. Wood and his assistant, Loomis [20] and was explored as a medical modality in 1938 by Raiman Pohlman at Charité University Hospital, Berlin. Pohlman demonstrated the therapeutic effects of ultrasonic waves in human tissues and went on to introduce ultrasonic physiotherapy as a routine procedure in medical practice (Fig. 4) [21].
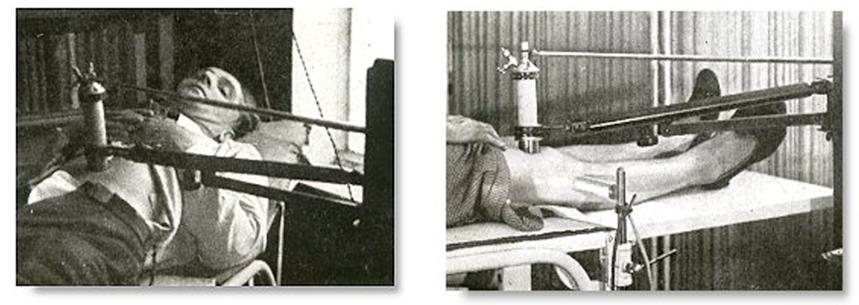
Fig. 4. Raiman Pohlman, early therapeutic ultrasound apparatus
Left: Treating a gastric ulcer. Right: Treating arthritis.
(From Les Ultra-sons appliques a la medecine. Andre Denier, 1951)
Рис. 4. Райман Полман, первоначальный терапевтический ультразвуковой аппарат. Слева: лечение язвы желудка. Справа: лечение артрита.
(Из книги «Медицинское применение ультразвука». Андре Денье, 1951)
Today, therapeutic ultrasound is typically applied at 1MHz, 2 MHz or 3MHz from a piezo-electric transducer, driven by an electronic oscillator and amplifier. Penetration depths of up to 5cm are achievable at 1MHz to support major physical trauma, while 2MHz and 3MHz frequencies are typically used to treat superficial conditions [22]. The therapeutic benefits of ultrasound are classified into thermal and non-thermal effects. With the discovery of ultrasound’s medical properties, research burgeoned and it is now established fact that ultrasound has effective medical properties: breaking up kidney stones via ultrasonic lithotripsy [23] shrinking tumours via high intensity focussed ultrasound (HIFU), histotripsy [24] targeted drug delivery [25] and reducing brain plaque [26] are a few examples of its many clinical applications. In hospitals and sports injury clinics throughout the world, therapeutic ultrasound is also used to support or accelerate the healing of soft tissues damaged by physical trauma, although the underlying biological healing mechanisms of therapeutic ultrasound remain poorly understood [27].
In 1928, Professor Erwin Schliephake, a German scientist who began his career at the Physiological-Chemical Institute in Leipzig, discovered that audible sounds create therapeutic effects (Fig. 5). His research inspired Mr. Lindacher, a colleague, to develop a hand-held, self-applied device that emits infra sonic vibrations [28].
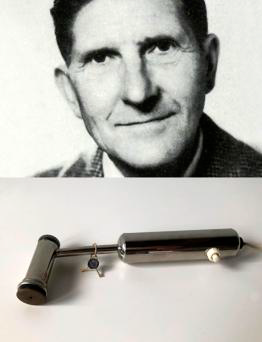
Fig. 5. Professor Erwin Schliephake, and his infrasonic device
Рис. 5. Профессор Эрвин Шлифаке и его инфразвуковой прибор
(https://novafon.com/en/history)
In the 1960s, English osteopath, Dr. Peter Guy Manners, developed an audible sound therapy modality that he named «Cymatic Therapy» that proved effective for the support of a wide range of ailments. («Cymatics» is derived from the Greek word «kyma» — meaning «wave» — and was coined by Swiss medical doctor, Hans Jenny.) In recent years, several manufacturers have developed audible sound therapy devices [29, 30, 31], one of whom is continuing the work of Dr. Manners. [31].
MUSIC THERAPY, MUSIC MEDICINE, AND SOUND THERAPY DEFINITIONS
Music Therapy is an accepted form of complimentary therapy in many hospitals and clinics, and may be defined as: «The clinical and evidence-based use of music interventions to accomplish individualized goals within a therapeutic relationship by a credentialed
professional who has completed an approved music therapy program» [32]. Music Therapy is a proven modality but is limiting in the sense that each patient requires a music therapist with whom to work. A plethora of books and scholarly articles are available on the subject of music therapy, and therefore is not the focus of this chapter.
Music Medicine may be defined as: «Listening to music [for the purpose of healing] without the presence of a therapist» [33].
Music Medicine is a relatively new clinical modality that refers to the therapeutic utilisation of music, chosen by the patient in a clinical setting without the intervention of a therapist. As its title implies, music medicine focuses on the demonstrable benefits of music as treatment for specific health challenges. The mechanisms by which music affects the body’s systems are complex and this chapter provide a short introduction into this subject.
Sound Therapy is defined by the International Sound Therapy Association as:
«The application of audible sound to the full body or to a specific part of the body, from electronically-generated sound sources, or from musical sources, as therapeutic support, by a credentialed Sound Therapy practitioner» [34]. This definition clarifies that therapeutic audible sound can be generated by electronic means, or provided by a musical source. The biological mechanisms triggered by such sonic support will be discussed later in this section of the chapter. Meta-analyses of Music Medicine in Clinical Trials A Cochrane analysis of twenty-six music medicine clinical trials with a total of 1,369 participants titled, Music for stress and anxiety reduction in coronary heart disease patients, concluded that «listening to music may have a beneficial effect on systolic blood pressure and heart rate in people with coronary heart disease and appears to be effective in reducing anxiety in people with myocardial infarction». The same report mentioned, «Listening to music may reduce pain and respiratory rate and appears to improve patients’ quality of sleep following a cardiac procedure or surgery» [35].
A study by the University of Belgrade School of Medicine, led by Dr. Predag Mitrovic, involved 350 patients diagnosed with a heart attack and early post-infarction angina. Half were randomly assigned to receive standard treatment while half were assigned to regular music sessions in addition to the standard treatment. Researchers fine-tuned the music selection by working with the patient to determine the optimal music tempo and tonality, therefore, the initial stage of the study would technically be classed as music therapy, while the major part of the study would, today, be classified as music medicine since the participants listened to music at home, without a therapist. Participants who listened to music reported less anxiety and less pain sensation than participants who received the standard treatment alone. Dr. Mitrovic concluded, «Sedative music was more effective than treatment in decreasing anxiety and pain in patients with HT [hypertension] and EPA [post-infarction angina]. Patients with HT should have the benefit of using sedative music as an adjuvant to medication during EPA episodes» [36].
Johns Hopkins Medicine also acknowledges the role of music in addressing illness and indicates a range of illnesses they intend to treat with music, including: Huntington’s Disease, Parkinson’s Disease, and Dementia [37]. McGill University in Montreal is also conducting studies in music medicine. In a meta-analysis of 400 studies, Dr. Daniel J. Levitin and Dr. Mona Lisa Chanda found that music improves the body's immune system function, reduces stress, and was found to be more effective than prescription drugs in reducing anxiety before surgery. They also found that listening to and playing music increases the body's production of the antibody immunoglobulin A and natural killer cells, boosting the immune system's effectiveness, as well as reducing levels of the stress hormone cortisol [38]. At Riuniti hospital in Ancona, Italy, neurosurgeon, Dr. Roberto Trignani performed an operation to remove a double tumour in the spinal cord of a ten-year-old boy, while molecular biologist and pianist, Emiliano Toso, played a grand piano in the operating theatre (Fig. 6).

Fig. 6. Dr. Emiliano Toso playing piano in an Operating Room, during live neurosurgery (photo courtesy of Dr. Emeliano Toso)
Рис. 6. Доктор Эмилиано Тосо играет на фортепиано в операционной во время нейрохирургической операции (фото любезно предоставлено доктором Эмилиано Тосо)
Monitoring the boy’s brain activity via an encephalogram, suggested that the boy perceived the music. Dr. Toso said, «We tried stopping then restarting the music, noticing the patient's response. Despite the fact that the boy was under total anaesthesia, his brain appeared to perceive the music and this was very exciting». Dr. Trignani, head of the neurosurgery unit of Riuniti Hospital, commented, «Everything went well, there were no complications and there was a magical atmosphere of complete harmony in the Operating Room» [39].
It is admirable and noble that musicians contribute their time and talent to playing in hospitals. The harp, in particular, has a long history of use in clinical settings and nursing homes and it is likely that it will always form an important aspect of patient care. However, to reach larger numbers of patients, and to give individual choice of music genre, a convenient solution is that of «modulated ultrasound speakers» [40, 41] which emit wavelengths of only a few millimetres, thus, the acoustic energy travels as a narrow beam. Ultrasound contains frequencies far beyond the range of human hearing and is completely inaudible. However, as the low energy ultrasonic beam travels through the air, the inherent properties of the air molecules within the beam give rise to frequency components in the audible band that can be heard only by the patient to whom the beam is directed. In this future scenario, the patient would choose the music that they prefer from a bedside console, and be beamed to them from an ultrasonic ceiling-mounted speaker. Adjacent patients would not hear the music. In the illustration, a patient is listening to music without headphones, yet the nurse cannot hear the music (Fig. 7).

Fig. 7. A patient listens to music without headphones and without disturbing the nurse or other patients (photo with graphic overlay by the author)
Рис. 7. Пациент слушает музыку без наушников и не беспокоя медсестру или других пациентов (фото с графической накладкой автора)
A brief overview of some of the biological mechanisms activated by full body immersion in music or in specific sound frequencies (Detailed explanations are provided later in the chapter.) Full body immersion in music or in specific sound frequencies (as distinct from listening with headphones), activates several beneficial biological mechanisms, five of which are briefly summarised as follows:
Enhances nitric oxide (NO) production through active and passive acoustic stimulation of the nasal cavities and lungs by specific sound frequencies and music, resulting in a broad range of health benefits. Promotes pain mediation through stimulation of the body’s large A-beta fibres or A-alpha fibres in the area experiencing pain, thus causing the pain ‘gate’ to close.
Increases the availability of oxygen binding to haemoglobin molecules by low frequency sound pressure, thus breaking the pain-spasm-pain cycle or ‘splinting cycle’ by increasing the availability of oxygen to affected tissues.
Activates the meridian system, via ‘sonopuncture’, with many health benefits, including pain mediation.
Increases the availability of oxygen binding to haemoglobin molecules by low frequency sound pressure, thus aiding tissue repair mechanisms.
A brief overview of some of the biological mechanisms activated by headphone listening to music, or listening to specific sound frequencies (Detailed explanations are provided later in part 2 of this article.)
Mediates pain by the «Descending Inhibition of Pain» system, also referred to as the «top-down» modulation of pain. Such effects can be initiated by music (or white noise) as a result of activating endogenous opioids.
Promotes stress reduction with consequent reduction in blood pressure and cortisol levels, and induces a state of joy with consequent increase in dopamine levels, leading to a proliferation of leukocytes, thus boosting immune system efficiency.
Stimulates the brain binaurally—by binaural beats—to create changes in brain state, with physiological benefits. The vagus nerve is stimulated, thus regulating internal organ functions, including digestion, heart rate and respiratory rate, as well as promoting vasomotor activity and anti-inflammatory effects. Specific very low (sub audible) frequencies may also be applied by full ear headphones, combined with music.
Each of these biological mechanisms will be discussed separately.
ACTIVE AND PASSIVE SONIC STIMULATION OF THE NASAL CAVITIES AND LUNGS
Before the subject of sonic stimulation of the nasal cavities and lungs is discussed, it is important to outline some of the natural health benefits of nitric oxide (NO), which is naturally produced in many areas of the body including the cilia in the nasal cavities and the alveoli in the lungs. NO reduces blood pressure by vasodilation [42] and many other health benefits are derived from this important molecule, for example: promotion of wound healing by cellular proliferation and angiogenesis [43] mediation of cutaneous oedema and inflammation, cytotoxic action against pathogens [44] increases cerebral blood flow and oxygenation to the brain [45] inhibits the aggregation of platelets within blood vessels thus helping prevent thrombotic events [46] supports reduction of pulmonary hypertension and chronic obstructive airway disease [47] (Fig. 8).
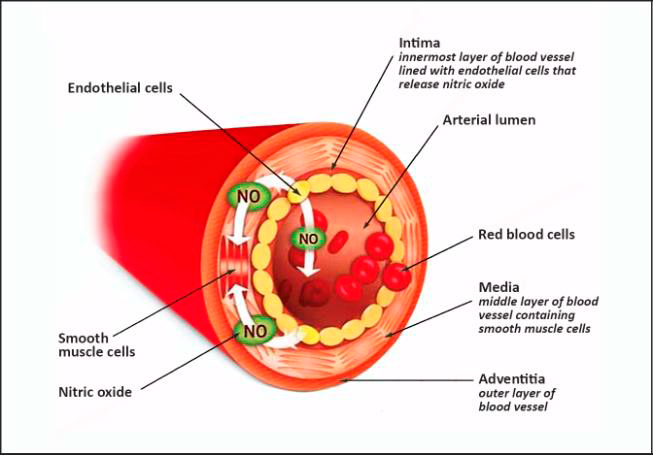
Fig. 8. Nitric oxide relaxes smooth muscle cells in the walls of blood vessels,
resulting in vasodilation (Courtesy of NIOX)
Рис. 8. Оксид азота расслабляет гладкомышечные клетки стенок сосудов, что приводит к расширению сосудов (с разрешения NIOX)
NO can be produced in the body from the inorganic nitrates in green leafy vegetables and from fruits, particularly by the oral microbiome [48] and is also stimulated by exercise [49] which can form part of a rehabilitation program, but the initial focus in this section is NO production in the nasal cavities brought about by both active and passive sonic stimulation. «Active» stimulation refers to the practise of vocal humming, which has been shown to greatly elevate NO production [50, 51]. The movement of air across the nasal cilia generates NO, from which the many health benefits are derived, although the exact mechanisms by which NO is produced by the nasal cilia is not fully understood [52].
The practise of nasal breathing is well known in the Yogic practise of pranayama, which means ‘breath control’ in Sanskrit, a practise that is mentioned in the Bhagavad Gita, written at some point between 400BCE and 200BCE [53].
In a paper titled «Assessment of nasal and sinus nitric oxide output using single-breath humming» [54] the authors show that NO is significantly increased by a single breath exhalation while humming, as shown in the graph (Fig. 9).
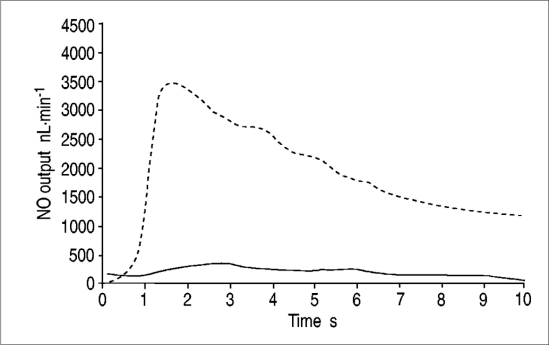
Fig. 9. Nitric Oxide levels during a single-breath nasal exhalation with (dotted line) and without humming (solid line) (Illustration from the paper: «Assessment of nasal and sinus nitric oxide output using single-breath humming exhalations».
Рис. 9. Уровни оксида азота при однократном энергичном носовом выдохе (пунктирная линия) и без усилия (сплошная линия) (Иллюстрация из статьи: «Оценка выработки оксида азота через нос и пазухи с помощью жужжащих выдохов на одном дыхании».
The authors of this study also carried out experiments to determine the optimum humming frequencies, and concluded that a measured frequency of 130Hz created the highest NO output of the sinus cavity in a human subject. The study does not specify whether the human subject was male or female but in either case the result is surprising when remembering that the sinuses consist of relatively small cavities, featuring Helmholtz resonant frequencies in the range 1kHz to 2kHz [55] depending on gender and maturity.
An interesting fact concerning this range of resonant frequencies concerns the ancient Egyptian use of the sistra instrument, the rattle with metal discs, mentioned in the introduction. At the Festival of Opet the sistra was used to stimulate the nostrils: «Receive the sistra presented to your nostril that he may give rejuvenating breath…» [19] a statement suggesting that the ancient Egyptians were aware that sistra emitted a specific quality of sound that caused a rejuvenating effect on the sinus cavities.
Adult female skulls and sinus cavities are typically smaller than those of adult males; smaller sinus cavities support higher resonant frequencies. It should also be remembered that humming does not generate a single frequency but gives rise to an array of harmonics and that the prime resonant mode of the sinus cavities is automatically «selected» during vocal humming as a natural aspect of Helmholtz resonance (the resonant property of a gas-filled cavity). Therefore, although the fundamental humming frequency of maximal excitation was found to be 130Hz, (in the study «Assessment of nasal and sinus nitric oxide output using single-breath humming») the sinus cavities would almost certainly have been excited by a specific harmonic of this frequency.
Nitric Oxide is also generated by the alveoli in the lungs [56] and can be stimulated by both active and passive sonic stimulation; actively by humming or singing, and passively by externally applied sonic frequencies or music. Indicators regarding the optimum frequencies for passive stimulation can be obtained from studies in which the respiratory system has been modelled in terms of its resonant sonic characteristics [57, 58]. In the study by University of Illinois [57] the Helmholtz resonant frequency of a healthy volunteer is shown to be in the order of 100Hz, increasing to around 250Hz for a person suffering from pulmonary fibrosis. These frequencies will vary between individuals due to gender and lung capacity as a function of the patient’s genetic makeup. Similarly, the Helmholtz resonant frequencies of the sinus cavities will vary between individuals.
Identifying the precise resonant frequencies of the patient’s lungs or nasal cavities is not necessary to offer therapeutic intervention if the practitioner applies either broadband white noise [59] or music to the patient. Both of these sound sources contain thousands of frequencies and Helmholtz resonance principles are such that a cavity will automatically «choose» the frequency from a broadband sound source at which the cavity is naturally resonant. In the case of white noise, this sound source can be filtered through a parametric equaliser [60] that facilitates the selection of specific bands of frequencies that are appropriate for stimulating either the lungs or sinus cavities. By such filtering of white noise, any unpleasant sensations associated with the noise experience can be minimized. White noise generators are commercially available from many manufacturers and the audio signal from the generator drives a conventional audio amplifier and speaker. The speaker(s) should offer a frequency response that covers the range needed, e.g., ideally as low as 20Hz for excitation of lungs, and as high as 2kHz for excitation of sinus cavities. Commercially manufactured reference monitor speakers, which are typically used in recording studios, are ideal for this purpose because they offer an extended low frequency response and are typically fitted with «tweeters» for reproduction of high frequencies.
These same principles in which a patient’s sinus cavities or lungs automatically choose the specific frequency at which the cavity is naturally resonant, also apply to many musical instruments, for example, harps and gongs, whether played live in a clinical setting or via high fidelity reproduction equipment (Fig. 10).
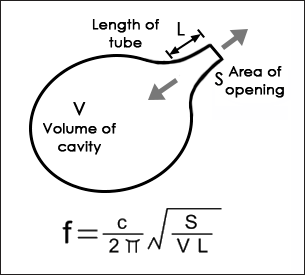
Fig. 10. Helmholtz Resonance
f = resonant frequency of cavity, c = speed of sound in air, S = area of opening,
V = volume of air in the cavity, L = length of the tube
Рис. 10. Резонанс Гельмгольц f = резонансная частота полости, c = скорость звука в воздухе, S = площадь отверстия, V = объем воздуха в полости, L = длина трубки
When applying recorded music to a patient for the purposes of lung and/or sinus activation, parametric filtering is not required because music provides a pleasant experience, assuming that the sound pressure levels are modest, e.g., 60 to 80dBA when measured in close proximity to the patient. The patient should make the music choice, although it is important that the music chosen contains a wide range of frequencies to ensure optimal stimulation of the lungs and sinus cavities.
In addition to stimulation of nitric oxide production, acoustic stimulation of the sinus cavities and lungs can also help to clear mucus and improves symptoms of Chronic Obstructive Pulmonary Disease (COPD) and chronic bronchitis [61].
In a 26-week randomised control trial the «Lung Flute» respiratory device, which produces a low frequency acoustic wave, the symptoms and health status of people with COPD and chronic bronchitis improved. The authors stated that mucus hypersecretion and impaired mucociliary clearance is prevalent in many patients with COPD, and contributes significantly to the morbidity and mortality of this disease, and concluded that the Lung Flute is a safe and effective treatment in COPD with chronic bronchitis [61].
CHRONIC PAIN MEDIATION BY AUDIBLE SONIC STIMULATION OF NOCICEPTORS
Pain is a vital function of the body, providing early warning of damage or potential damage. It is both a sensory and emotional experience, affected by psychological factors such as past experiences, beliefs about pain, fear or anxiety [62]. Tissue injury, for example, initiates the liberation of various inflammatory mediators, including prostaglandins, cytokines and chemokines. Leukocyte migration to the injured area, a characteristic of the inflammatory response, is associated with pain and tenderness, and is involved in wound healing [63]. Acute pain is well understood and can be successfully mediated by analgesic medications; it is not within the scope of this chapter. Chronic pain is a common, complex, and distressing problem, which has a significant impact on individuals and society [64]. Chronic pain, like most diseases, often arises from a series or combination of multiple events [64]. The biological processes that lead to the chronic pain state further increase sensitivity to painful stimuli and perceived levels of stress, which further modifies pain-related gene expression, creating a pathological pain cycle [65]. Even when there is a solitary precipitating event in the genesis of chronic pain (e.g. injury), there remain a series of factors that affect the duration, intensity, and effects (physical, psychological, social, and emotional) of chronic pain [64]. The International Association for the Study of Pain, define pain as «An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential damage» [66] and chronic pain is «pain which has persisted beyond normal tissue healing time» [67]. Pain is regarded as chronic when it has lasted for more than three to six months [68]. Considering that pain is a universal experience, it is not understood why only a relatively small proportion of humans develop a chronic pain syndrome [69]. Prolonged use of analgesics, such as chronic opioid therapy, is associated with constipation, sleep-disordered breathing, hypothalamic-pituitary-adrenal dysregulation, fractures (as a result of osteoporosis) and significant declines in health-related quality of life and increased health care costs [70]. Therefore, it would be advantageous to mitigate chronic pain without long term use of analgesics. In this section we discuss audible sonic stimulation of the body’s nociceptors, as an alternative therapeutic modality in the treatment of chronic pain. Unlike prolonged use of analgesics, audible sonic interventions have no known adverse side effects. Nerve signal conduction by sound To lay a foundation for discussion in the principles of pain mediation by sound, it is important to mention discoveries concerning nerve signal transmission by sound.
In 1952, Alan Hodgkin and Andrew Huxley, working with a squid’s giant axons, described how action potentials (or nerve impulses) in neurons are initiated and propagated, known today as the Hodgkin–Huxley model [71]. It is regarded as one of the great achievements of twentieth century biophysics, for which they received the Nobel Prize in Medicine in 1963. Their theory, involving the flow of electric currents in nerves, became the standard teaching model in medical and biology textbooks. However, one aspect that puzzled researchers was the relatively slow conduction speeds in nerves, when compared with conduction speeds of electric currents in conductors. The speed of light in vacuum is 2.998 × 108 metres per second, which is approximately equal to a distance of 30cm per nano second. The speed of an electrical signal in a coaxial cable is about 2/3 of this, or 20cm per nano second, therefore, in one second the signal in a coaxial conductor will travel approximately 200,000,000 metres, which equates to a little over half the distance between the earth to the moon.
Nerve fibres, by comparison conduct signals several orders of magnitude slower than that of coaxial cables. The highest conduction speeds for nerve fibres are those of muscle axons, which can achieve speeds of over 100 metres per second.
The comparison with coaxial cables is made because in the four main classifications of primary afferent nerve fibres, three of them (A Alpha, A Beta and A Delta) are myelinated, meaning that the nerve axon is enclosed in a myelin sheath, therefore resembling the dielectric material of a coaxial cable. Type Cnerve fibre is unmyelinated, resembling a single electrical conductor. With coaxial cables, the speed of conduction is a function of the diameter of the fibre and the diameter of its outer sheath, and this is similar for myelinated nerve fibres; the larger fibres feature higher conduction speeds (Fig. 11).
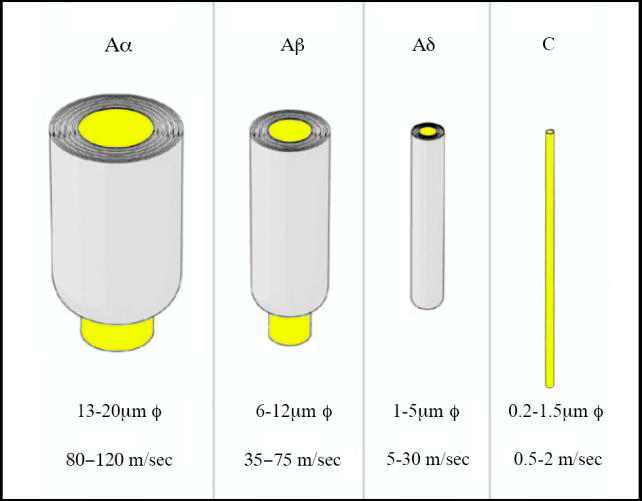
Fig. 11. The main classifications of afferent nerve fibres and their conduction speeds, which are very slow compared with electric currents in coaxial cables (Illustration by the author)
Рис. 11. Классификация основных афферентных нервных волокон и скорости проведения нервных импульсов, которые значительно медленнее скорости проведения электрических токов в коаксиальных кабелях
(Иллюстрация автора)
However, in 2005 a new model of nerve conduction was proposed by researchers at the Niels Bohr Institute at the University of Copenhagen, whose experiments showed that nerves conduct sound (soliton impulses), which in turn generate electrical pulses, due to the piezo electric effect [72]. In their paper they note that «…measured propagation velocities, which are ~100 m/s in myelinated nerves, find a satisfying explanation». Put differently, propagation of nerve impulses by sound explains the slow conduction speeds, while such sonic impulses give rise to electrical impulses that travel to the brain for interpretation. Sonic propagation of nerve signals was first proposed by Konrad Kaufmann, in a 1989 unpublished paper [73]. Other researchers have found similar results, supporting the Neils Bohr Institute findings to a large degree [74, 75]. This discovery has significant implications for sound therapy and music medicine, particularly for whole body immersion in music and specific sound frequencies.
Principles of pain mediation by sound Nociceptors are the specialised sensory receptors responsible for the detection of noxious (unpleasant) stimuli, transforming the stimuli into electrical signals, which are then conducted to the central nervous system [62]. They are the free nerve endings of primary afferent fibres and are distributed throughout the tissues of the body, including the skin, viscera, muscles, joints and the meninges of the brain, (though not in the grey matter of the brain). The four main classifications of afferent fibre have specialised roles, for example, response to light touch, or to acute events, or response to chemical or thermal stimuli, but crucially all types of afferent nerve fibre respond to mechanical pressure. And since sound may be defined as: «Mechanical radiant energy that is transmitted by longitudinal pressure waves in a material...» [76], it becomes clear that all types of afferent fibre respond to sound. This fact is reinforced by the Niels Bohr Institute discovery that nerves conduct sound as soliton pulses. When nociceptors are stimulated, nerve impulses are transmitted to three spinal cord systems: the cells of the substantia gelatinosa in the dorsal horn; the dorsal-column fibers that project toward the brain; and the first central transmission (T) cells in the dorsal horn [77] (Fig. 12).
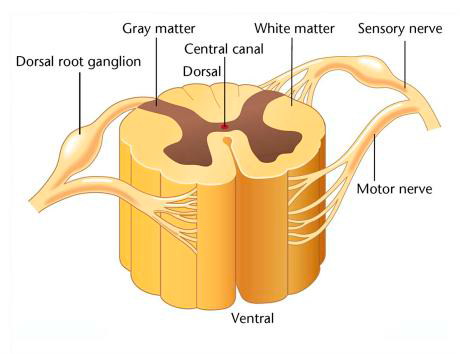
Fig. 12. Cross section through spinal column showing the dorsal root ganglion (Graphic: Emri Terim) Рис.12. На поперечном срезе позвоночника, показан
ганглий дорсального корешка
(Изображение: Эмри Терим)
The theory by which sound frequencies can mediate pain are based on the «Gate Control Theory of Pain», which was first proposed in 1965 by Ronald Melzack and Patrick Wall [77]. The theory was initially met with skepticism, but despite having to undergo several modifications, its basic conception remains unchanged. Their theory provides a physiological-neural explanation for pain perception and ultimately revolutionized pain research. Gate Control Theory proposes that there are gates between the afferent nerves and the brain, located in the spinal column, which control how pain messages flow from the peripheral nervous system to the central nervous system. For example, pain-signals conduct freely along small A-delta afferent fibres (that sense sharp pain) and small type C afferent fibres (that sense dull pain) open the gate, resulting in the perception of pain in the brain. By stimulating the large A-beta fibres or A-alpha fibres in the area experiencing pain, a reaction is caused in nearby inhibitory neurons. Once activated, Inhibitory Neurons, which sit on the same path as the Projection Neurons, the gate closes, thus muting pain signals before they reach the brain. Stimulating A-beta fibres or A-alpha fibres can be achieved by specific sound frequencies, as mentioned below (Fig. 13). Fig. 13.
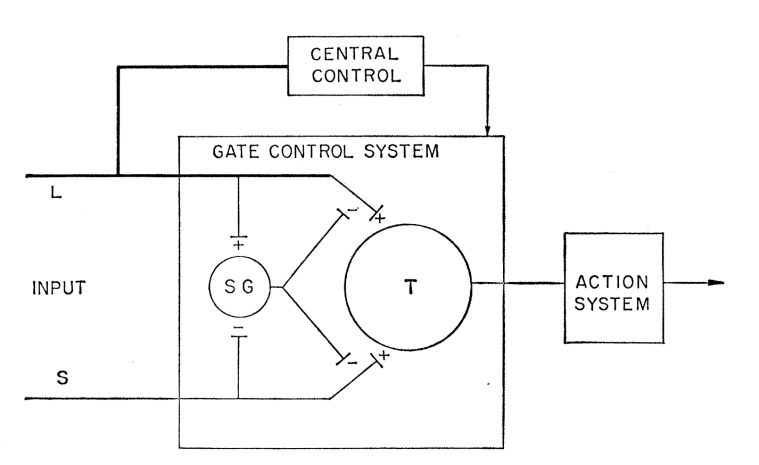
Fig. 13. The Melzack-Wall Gate Control System (from Melzack and Wall) L = large diameter nerve fibers, S = small diameter nerve fibers. The fibers project to the substantia gelatinosa (SG) and first central transmission (T) cells. Activity in large fibers inhibits signals from small fibers. (Drawing from Ronald Melzack & Patrick Wall «Pain Mechanisms: A New Theory»)
Рис. 13. Система управления воротами Melzack-Wall (от Мелзака и Уолла)
L = нервные волокна большого диаметра, S = нервные волокна малого диаметра. Волокна проецируются на желатинозную субстанцию (SG) и первые центральные трансмиссионные (T) клетки. Активность крупных волокон подавляет сигналы от мелких волокон.
(Рисунок из книги Р. Мелзака и П.Уолла «Механизмы боли: новая теория»)
Some of the optimal frequencies found to be beneficial for pain mediation via nociceptor stimulation were discovered in Finland by clinical psychologist, Petri Lehikoinen, in the range 27Hz to 113Hz. Lehikoinen developed a therapeutic system: Physio Acoustic Sound (PAS) therapy, that was approved in the USA by the Federal Drug Administration (FDA) and in the UK by the British Standards Institute (BSI) for three claims: decreased pain, increased blood and lymphatic circulation and increased muscle relaxation and mobility [78]. In Norway, Olav Skille placed particular emphasis on specific therapeutic frequencies at 40Hz, 52Hz, 68Hz and 86Hz [78].
Vibratory analgesia was also studied by Salter and Henry, examining P1-purinergic receptors in the dorsal horn by adenosine, the neurotransmitter. In their study with cats, sound at 80Hz induced depression of lower lumbar nociceptive neurons, which remained affected for up to four hours after cessation of the sound. The depression of the neurons revealed that adenosine was responsible for the analgesic effect, suggesting that gate control may be mediated by the release of adenosine resulting from the application of sound [78].
Whole Body Vibration (WBV) is also becoming a popular therapy for low back pain and to improve functional abilities of patients, however the term “Whole Body Vibration” appears to be something of a misnomer in the sense that it has come to mean vibration applied specifically via the feet, that is, a vibrating platform of which the patient stands.
However, WBV can be adapted to use in beds, as mentioned below. From seven randomized control trials involving 418 patients, four studies using pain as an outcome measure showed that WBV had a beneficial effect on pain compared with the control group [79].
Although current WBV platforms can produce vibration frequencies up to 100Hz, frequencies below 30Hz are most commonly used [78].
Apart from their use in pain mediation and pain management, WBV deployed via a bed can support patients in an Intensive Care Unit (ICU). Critical illnesses can lead to a mean weight loss of 17% within the first 10 days of stay in the intensive care unit and up to 40% within 4–6 weeks.
Early mobilization has a variety of beneficial effects, including mobility, reduced risk of venous thromboembolism, pneumonia, in addition to socioeconomic advantages.
Effective active rehabilitation requires a conscious patient who is willing to participate, whereas WBV can be applied passively in bed [80] (Fig. 14).

Fig 14. Whole Body Vibration
Deployed to the patient by fixing the device to the foot of the bed
(Courtesy of German Centre for Lung Research)
Рис. 14. Вибрация всего тела. Размещается на пациенте путем фиксации устройства к изножью кровати
(Фото любезно предоставлено Немецким центром исследований легких)
The WBV device was attached to the foot of the patient’s bed, thus inducing vibrations into the bed frame. The patient lay in the supine position and the bed was inclined by 25° to transmit a sufficient load to the patient’s lower limbs. Many beneficial health parameters were reported in the study but crucially, a significant increase in the patients’ oxygen saturation level (SaO2) was seen in the second period, between the first and second minute [81]. This increase in oxygen binding to haemoglobin molecules by low frequency sound may have important implications for pain, as mentioned below, in the section: Breaking the ‘pain-spasm-pain’ cycle in spinal injury.
In a study titled, The Effects of Long-Term 40Hz Physioacoustic Vibrations on Motor Impairments in Parkinson’s Disease: A Double-Blinded Randomized Control Trial, the authors focussed on testing the efficacy of 40Hz vibrations in support of Parkinson’s disease, a progressive neurodegenerative disorder. Symptoms are typically characterised by tremor, rigidity, bradykinesia and postural instability [81]. 40Hz was chosen because among the range of gamma frequencies (25-140Hz) it has shown consistent evidence for neuroprotection. The physioacoustic therapy employed was that of special reclining chairs with built in low frequency transducers. The 40Hz audio signal was inputted to the chairs using a scanning technique that caused the frequency to vary between 39.96Hz and
40.06Hz, resulting in a kinaesthetic pulsating effect. The placebo control group also sat in a reclining chair band heard a 40Hz tone without receiving any bodily vibrations.
The twelve-week course was completed by twenty-one participants in the treatment group and fifteen participants in the placebo group and both groups were not significantly different at baseline in age or motor symptom severity. The authors found that 40Hz vibration administered by the special chair (which literally induces uniform vibration throughout the body, as distinct from WBV platforms that induce vibration only via the feet) was found to significantly reduce overall motor symptoms of Parkinson’s disease [81]. The authors suggested that the most viable mechanism for the efficacy of low frequency vibration is that it may act to disrupt the pathological oscillatory activity within basal ganglia-thalamocortical circuits. The vibration transmitted throughout the entire body may act to perturb abnormally synchronised oscillations, in addition to eliciting supplementary releases of endogenous dopamine [81].
Neurogenic pain Pain can also be experienced that is not a consequence of nociception, categorized as ‘neurogenic’ pain, stemming from neural circuit dysrhythmias or disconnections [78]. However, neurogenic pain has been found to be mediated by vibratory analgesia as a result of cortical dynamics [82]. For example, in a study with fibromyalgia patients, positive effects were obtained due to oscillatory coherence, with 40Hz vibro-tactile stimulation of the body [83].
Another vibro-tactile study mentioned that patients with chronic pain syndromes, such as fibromyalgia, complain of widespread pain and tenderness, as well as non-refreshing sleep, cognitive dysfunction, and negative mood. Several lines of evidence implicate abnormalities of central pain processing as contributors for chronic pain, including dysfunctional descending pain inhibition [84]. Their study enrolled 28 normal pain-free controls, 29 fibromyalgia patients, and 19 subjects with neck or back pain. Pain was administered to all subjects via sensitivity-adjusted heat stimuli to each forearm and pain intensity was noted using a mechanical visual analogue scale (VAS). Subsequently, the 100Hz vibrating probe, with a round footplate (diameter 4cm) was placed either on the same forearm next to the heat stimulus or on the forearm opposite to the heat stimuli. The authors concluded that vibro-tactile stimulation effectively recruited analgesic mechanisms not only in normal pain free controls, but also in patients with chronic musculoskeletal pain, including fibromyalgia [84]. The descending inhibition of pain by music and white noise
A second mechanism of pain mediation, sometimes referred to as the «top down» modulation of pain [85] but more accurately described as the «Descending Inhibitory system» [86] or «Descending Analgesia System» [87] can be activated by music that creates a strong emotional response. Such music-invoked emotions can be described as «thrills» [88].
Music offers a wealth of benefits with no negative side effects and is, therefore, a favourable option for those who are looking for alternative pain management therapies [86].
The origin of this second pain mediation mechanism arose from an early study by Dr. Henry K. Beecher, titled «Pain in men wounded in battle» in which he notes, «Three-quarters of badly wounded men, although they have received no morphine for a matter of hours have so little pain that they do not want pain relief medication… Strong emotion can block pain» [89].
Descending Inhibition concerns tracts arising from the brainstem that terminate on the spinal cord to suppress sensory transmission and consequently produce analgesia [86] (Fig. 15).
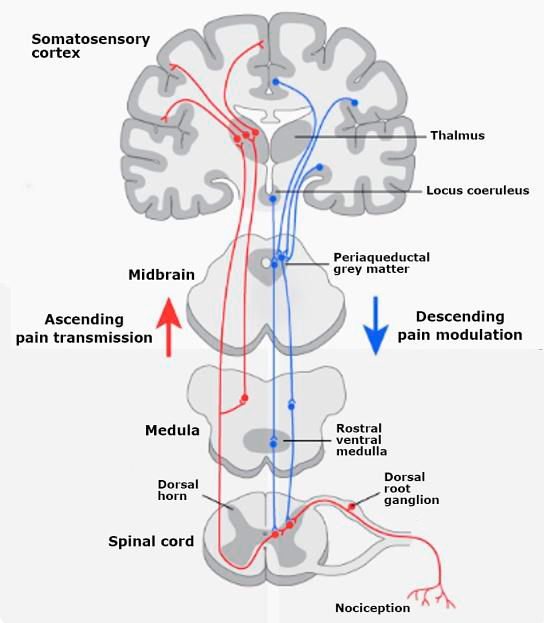
Fig. 15. Ascending and Descending Pain Pathways
(Illustration courtesy of walterskluwer.com)
Рис. 15. Восходящие и нисходящие пути боли (Фото предоставлено walterskluwer.com)
Music induced analgesia is hypothesized to occur as a result of the release of opioids during music listening [87, 88] thereby engaging the descending analgesia system that creates anti-nociceptive responses in the spinal cord. Descending inhibitory pathways use endogenous opioids, hydroxytryptamine (5-HT) and noradrenaline and their effects are mediated through supraspinal, midbrain-spinal and brainstem-spinal circuits. [90] A large number of brainstem structures suppress pain through descending projections to the spinal dorsal horn, and in most cases their descending pain suppressive effect is relayed through the periaqueductal gray matter (PAG) and the rostral ventromedial medulla (RVM). [86] The RVM in the brainstem is a particularly important relay site for integrating descending influences to the spinal cord [86].
In an early (1960) seminal paper on this subject, titled “Suppression of Pain by Sound”, by Gardner, Licklider and Weisz, the authors refer to “Audio Analgesia”. They mention that in about 90% of 5,000 dental operations, including tooth extractions, sound stimulation was the only analgesic agent required.[91] Patients wore headphones and listened to relaxing music before the dental procedure. During the procedure the headphones were fed with white noise. The intensity of white noise used in these procedures was reported in another early paper (1962) The Effects of White Sound and Music upon the Superficial Pain Threshold by Robson and Davenport, to be as high as 120 decibels [92]. A foot switch was used by the dentist to lower the sound level to enable communication with the patient by an external microphone. The reported 120 decibels was believed to “not damage hearing when used for relatively short periods”, however, by today’s safety standards this is a dangerous sound level and long or repeated exposure to sound at or above 85 dBA can cause hearing loss. [93] (A-weighted decibels). However, the fact that so many dental operations were accomplished without the use of injected analgesics is impressive and suggests that trials of white noise at 85dBA should be conducted, to assess if this safe level is efficacious as a descending analgesia substitute to music.
In the study: «Music Modulation of Pain Perception and Pain-Related Activity in the Brain, Brain Stem, and Spinal Cord: A Functional Magnetic Resonance Study», the authors concluded that when pain was administered [by a well- characterised thermal method] to female participants, who were asked to select their favourite music of any genre, perceived pain ratings were significantly reduced in activity in brain regions that process music and pain modulation [87]. Brain stem and spinal cord structures showed similar activity changes concurrent with descending modulation, demonstrating activation of the PAG region with corresponding suppression within the dorsal horn region [87]. The authors also concluded that endogenous opioids may exert widespread analgesic effects by influencing several brain and brain stem regions within the descending analgesia pathway [87].
This is the end of part 1 of this article. In part 2 we will explore the pain-spasm-pain cycle; pain relief and anxiety relief by acupressure and sonopuncture; pain relief by sonopuncture administered by electronic devices; oxygen-driven healing by sound, musical stimulation of the immune system (via headphones or full body immersion); binaural Beats (via headphones) to create changes in brain state, with physiological benefits; sonic stimulation of the vagus nerve (via headphones) and by vocalisations, and the future of vibrational medicine.
1. Rubik B. The Biofield Hypothesis: Its Biophysical Basis and Role in Medicine. The Journal of Alternative and Complementary Medicine, Vol 8, No 6. DOI;https://doi.org/10.1089/10755530260511711
2. When Microbial Conversations Get Physical, Gemma Reguera, Trends in Microbiology, DOI:https://doi.org/10.1016/j.tim.2010.12.007
3. Das Wesen der Materie [The Nature of Matter] speech at Florence, Italy (1944) (from Archiv zur Geschichte der Max-Planck-Gesellschaft, Abt. Va, Rep. 11 Planck, Nr. 1797).
4. The Institute for Functional Medicine. Available at: https://www.ifm.org/ functional-medicine/
5. Available at: https://courses.lumenlearning.com/physics/chapter/17-3-sound-intensity-and-sound-level/
6. Vatansever F. and Hamblin M.R. Far Infrared radiation (FIR): its biological effects and medical applications. Photonics and Lasers in Medicine. 2012 Nov 1;4: 255-266. DOI:https://doi.org/10.1515/plm-2012-0034
7. The Mereon Matrix, editors, McNair J.B., Dennis L., and Kauffman, L. p783-809: Reid J.S., The Emergent Science of Cymatics. World Scientific, ISSN 0219-9769. ISBN: 978-981-3233-55-3.
8. Life of Pythagoras, Iamblichus, Taylor T. Translated from the Greek, p. 7. Inner Traditions. (Iamblichus was a Syrian philosopher who lived circa 325 to circa 245 BC; therefore, a period of 170 years separates Pythagoras’ death from Iamblichus’ birth.)
9. The Athenian, Isocrates (436-338 BC), in his book Busiris, mentioned Pythagoras’ travels in Egypt: Measuring Heaven: Pythagoras and his influence on thought and art in antiquity and the Middle Ages, Christiane L. Joost-Gaugier.
10. The Life of Pythagoras, Professor Moritz Cantor, Heidelberg, Germany. Open Court Magazine, Volume 6, Number 493, June 1897.
11. Pythagoras: His Life and Teaching, a Compendium of Classical Sources, Thomas Stanley, Ibis Press.
12. Thaut M.H. Music as therapy in early history. Progress in Brain Research, Vol 217, DOI:https://doi.org/10.1016/bs.pbr.2014.11.025
13. Nunn J.F. Ancient Egyptian Medicine, British Museum Press, 1997. p111 and p122. ISBN: 0-7141-1906-7
14. Lipton B. The Biology of Belief. Elite Books, 2005. ISBN: 0-9759914-7-7
15. Schwaller de Lubicz R.A. Sacred Science. Inner Traditions, Bear & Co, 1989. ISBN: 10:0892812222
16. Aristotle. Poetics. Loeb Classical Library. p395. ISBN: 0-674-99563-5
17. The Corpus Hermeticum, p74. Translated by Salaman C,. Oyen D., & Wharton, W.D. Gerald Duckworth & Co. Ltd, 1999. ISBN: 0-7156-2939-5
18. Imhotep. Available at: https://www.worldhistory.org/imhotep/
19. Manniche, L. Music and Musicians in Ancient Egypt. p72. British Museum Press, 1991. ISBN: 0-7141-0949-5
20. Therapeutic ultrasound: some historical background and development in knowledge of its effect on healing: https://www.ncbi.nlm.nih.gov/ pubmed/25026107
21. Mason T.J. Therapeutic ultrasound, an overview. Journal of Ultrasonics Sonichemistry, 2011; 18 (4): 847-852. DOI:https://doi.org/10.1016/j.ultsonch.2011.01.004
22. Therapeutic Modalities for Allied Health Professionals. William E. Prentice. P271. McGraw-Hill publishing, p. 270.
23. Marberger, M, et al. Late Sequelae of Ultrasonic Lithotripsy of Renal Calculi. The Journal of Urology. DOI:https://doi.org/10.1002/jum.15191
24. Dubinsky J.D, at al. Histotripsy: The Next Generation of High-Intensity Focused Ultrasound for Focal Prostate Cancer Therapy. DOI:https://doi.org/10.1002/jum.15191
25. Tian Y. at al. New Aspects of Ultrasound-Mediated Targeted Delivery and Therapy for Cancer. Dove Press Open Access Journal. https://doi.org/10.2147/IJN.S201208
26. Nicodemus N.E. et al. Focused transcranial ultrasound for treatment of neurodegenerative dementia. Alzheimer’s & Dementia: Translational Research & Clinical Interventions, Volume 5, 2019, p374-381. DOI:https://doi.org/10.1016/j.trci.2019.06.007
27. Available at: http://www.electrotherapy.org/modality/ultrasound-therapy? highlight=over vieww#Therapeutic%20Ultrasound%20Thermal% 20and% 20 Non %20Thermal%20Effects%20Overview
28. Novasonic. Available at: https://novafon.com/de/historie
29. Medsonix. Available at: http://www.medsonix.com
30. KKT International. Available at: http://www.kktspine.com
31. Cyma Technologies Inc. Available at: http://cymatechnologies.com
32. American Music Therapy Association. Available at: https://www.musictherapy. org/about/
33. Brad J, et al. The impact of music therapy versus music medicine on psychological outcomes and pain in cancer patients: a mixed methods study. Support Care Cancer. DOI:https://doi.org/10.1007/s00520-014-2478-7
34. International Sound Therapy Association. Available at: http://istasounds.org/ about-us/about/
35. Available at: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858. CD006577.pub3
36. Available at: https://www.acc.org/about-acc/press-releases/2020/03/18/09/02/ music-as-medicine-30-minutes-a-day-shows-benefits-after-heart-attack
37. Available at: https://www.hopkinsmedicine.org/center-for-music-and-medicine/ music-as-medicine.html
38. Available at: https://www.mcgill.ca/newsroom/channels/news/major-health-benefits -music-uncovered-225589
39. Available at: https://www.reuters.com/article/us-italy-hospital-piano-idUSKBN27X2HU
40. Available at: https://www.holosonics.com/
41. Available at: https://ultrasonic-audio.com/
42. Cockroft J. Exploring vascular benefits of endothelium-derived nitric oxide Medicine. American Journal of Hypertension. DOIhttps://doi.org/10.1016/J.AMJHYPER. 2005.09.001
43. Majida R. et al. Nitric Oxide and Wound Healing. World Journal of Surgery. DOI:https://doi.org/10.1007/s00268-003-7396-7
44. Moilanen E. and Vapaatalo, H. Nitric oxide in inflammation and immune response. Annals of Medicine. DOI:https://doi.org/10.3109/07853899509002589
45. Noboru T, et al. Cerebral Blood Flow Regulation by Nitric Oxide: Recent Advances. Pharmacological Reviews. DOI:https://doi.org/10.1124/pr.108.000547
46. Loscalzo J. Nitric Oxide Insufficiency, Platelet Activation, and Arterial Thrombosis. Circulation Research. DOI:https://doi.org/10.1161/hh0801.089861
47. Ashutosh K, et al. Use of nitric oxide inhalation in chronic obstructive pulmonary disease. Thorax Journal. DOI:https://doi.org/10.1136/thorax.55.2.109
48. Jones A, et al. Dietary Nitrate and Nitric Oxide Metabolism: Mouth, Circulation, Skeletal Muscle, and Exercise Performance. Medicine and Science in Sports and Exercise. DOI:https://doi.org/10.1249/MSS.0000000000002470
49. Majorana A, et al. Exercise and the Nitric Oxide Vasodilator System. Sports Medicine. DOI:https://doi.org/10.2165/00007256-200333140-00001
50. Weitzberg E. and Lundberg J.O. Humming Greatly Increases Nasal Nitric Oxide.
51. Goldman J. and Goldman A. The Humming Effect. https://www.goodreads. com/book/show/32071037-the-humming-effect
52. Lundberg J.O. and Weitzberg E. Nasal nitric oxide in man. Thorax Journal. dx.doi.org/10.1136/thx.54.10.947
53. Available at: https://www.worldhistory.org/timeline/Bhagavad_Gita/
54. Maniscalco M. et al. Assessment of nasal and sinus nitric oxide output using single-breath humming exhalations. European Respiratory Journal. 2003; 22:323-329. DOI:https://doi.org/10.1183/09031936.03.00017903
55. Masuda S., Role of the maxillary sinus as a resonant cavity. DOI:https://doi.org/10.3950/jibiinkoka.95.71
56. Pietropaoli A.P., et al., Simultaneous Measurement of Nitric Oxide Production by Conducting and Alveolar Airways of Humans. American Physiological Society.
57. Henry B. and Royston J. T., A Multiscale Analytical Model of Bronchial Airway Acoustics, Department of Bioengineering, University of Illinois. DOI:https://doi.org/10.1121/1.5005497
58. Bogomolov A.V., et al. Mathematical Model of Sound Absorption by Lungs with Acoustic Stimulation of the Respiratory System. Doklady Biochemistry and Biophysics.2019; 487(1):247-250. DOI:https://doi.org/10.1134/S160767291904001X
59. White Noise definition: https://www.britannica.com/art/white-noise-music
60. Parametric Equaliser: https://www.presonus.com/learn/technical-articles/What-Is-a-Parametric-Eq
61. Sethi S., et al., Lung Flute Improves Symptoms and Health Status in COPD with Chronic Bronchitis: A 26 week randomised controlled trial. Clinical and Translational Medicine. DOI:https://doi.org/10.1186/s40169-014-0029-y
62. Reddi, D. et al. An introduction to pain pathways and mechanisms. British Journal of Hospital Medicine. DOI:https://doi.org/10.12968/hmed.2013.74.Sup12.C188
63. Wang X-M et al. Up-Regulation of IL-6, IL-8 and CCL2 Gene Expression After Acute Inflammation: Correlation to Clinical Pain. Pain Journal. 2009 Apr; 142(3): 275-283. DOI:https://doi.org/10.1016/j-pain.2009.02.001
64. Mills E.E.S. et al. Chronic pain: a review of its epidemiology and associated factors in population-based studies. British Journal of Anaesthesia. DOI:https://doi.org/10.1016/j.bja.2019.03.023
65. Diatchenko L. et al. The phenotypic and genetic signatures of common musculoskeletal pain conditions. Nature Reviews Rheumatology. 2013; 9(6). DOI:https://doi.org/10.1038/nrrheum.2013.43
66. Raja N., et al. The revised International Association for Study of Pain definition of pain: concepts, challenges, and compromises. Pain Journal. DOI:https://doi.org/10.1097/j.pain.0000000000001939
67. Bonica J.J. The management of pain. Philadelphia: Lea & Febiger, 1953.
68. Merskey H., Bogduk N. Classification of chronic pain. 2nd ed. Seattle: IASP Press, 1994. p. 1.
69. Rodriguez-Raecke R., et al. Brain gray matter decrease in chronic pain is the consequence and not the cause of pain. J Neurosci. 2009;29:13746-13750. DOI:https://doi.org/10.1523/JNEUROSCI.3687-09.2009
70. Baldini A. et al. A Review of Potential Adverse Effects of Long-Term Opioid Therapy: A Practitioner’s Guide. The Primary Care Companion for CNS Disorders. DOI:https://doi.org/10.4088/PCC.11m01326.
71. Schwiening C.J. A brief historical perspective: Hodgkin and Huxley. The Journal of Physiology. DOI:https://doi.org/10.1113/jphysiol.2012.230458
72. Heimburg T. and Jackson A.D. On soliton propagation in biomembranes and nerves. Proceedings of the National Academy of Sciences of the United States of America. DOI:https://doi.org/10.1073/pnas.0503823102
73. Kaufmann K. (1989). Action Potentials and Electrochemical Coupling in the Macroscopic Chiral Phospholipid Membrane. Caruaru, Brazil.
74. Shrivastava S. and Schneider M. F. Evidence for two-dimensional solitary sound waves in a lipid controlled interface and its implications for biological signalling. The Royal Society Publishing Interface. DOI:https://doi.org/10.1098/rsif.2014.0098
75. Shrivastava S. et al. Collision and annihilation of nonlinear sound waves and action potentials in interfaces. The Royal Society Publishing Interface. DOI:https://doi.org/10.1098/rsif.2017.0803
76. Available at: https://www.merriam-webster.com/dictionary/sound
77. Melzack R. and Wall P. Pain Mechanisms: A New Theory. Science, Volume 150, Number 3699.
78. Bartel L. and Mosabbir A. Possible Mechanisms for the Effects of Sound Vibration on Human Health. Healthcare, 2021, 9, 597. DOI:https://doi.org/10.3390/healthcare9050597
79. Wang W. et al. Efficacy of whole-body vibration therapy on pain and functional ability in people with non-specific low back pain: a systematic review. BMC Complementary Medicine and Therapies. (2020) 20:158 DOI:https://doi.org/10.1186/s12906-020-02948-x
80. Boeselt T. et al. Whole-body vibration therapy in intensive care patients: A feasibility and safety study. Journal of Rehabilitation Medicine. Vol 48, Issue 3.
81. Mosabbir A., et al. The Effects of Long-Term 40Hz Physioacoustic Vibrations on Motor Impairments in Parkinson’s Disease: A Double-Blinded Randomized Control Trial. Healthcare, 2020. DOI:https://doi.org/10.3390/healthcare8020113
82. Hollins M. et al. How does vibration reduce pain? Perception 2014; 43:70-84.
83. Naghdi L. et al. The effect of low-frequency sound stimulation on patients with fibromyalgia: A clinical study. Pain Res. Manag. 2015; 20: E21-e27.
84. Staud R. et al. Attenuation of Experimental Pain by Vibro-Tactile Stimulation in Patients with Chronic Local or Widespread Musculoskeletal Pain. European Journal of Pain. 2011; 15(8): 836-842. DOIhttps://doi.org/10.1016/j.ejpain.2011.01.011.
85. Urien L. and Wang J. Top-Down Cortical Control of Acute and Chronic Pain. Psychosomatic Medicine. 2019;81(9):851-858. DOIhttps://doi.org/10.1097/PSY.0000000000 000744
86. Pertovaara A. and Almedia A. Endogenous Pain Modulation. Chapter 13. Descending Inhibitory Systems. Handbook of Clinical Neurology, Vol. 81 (3rd series. Vol 3.) Pain. F. Cervero and T.S. Jenson, Editors. 2006, Elsevier.
87. Dobek C. et al. Music Modulation of Pain Perception and Pain-Related Activity in the Brain, Brain Stem, and Spinal Cord: A Functional Magnetic Resonance Imaging Study. The Journal of Pain. 2014; 15(10):1057-1068. DOI:https://doi.org/10.1016/j.jpain.2014.07.006.
88. Goldstein A. Thrills in response to music and other stimuli. Physiological Psychology. 1980; 8 (1):126-129. DOI:https://doi.org/10.3758/BF03326460
89. Beecher H.K. Pain in men wounded in battle. Annals of Surgery. 1946; 123(1): 96-105.
90. Susuki R. et al. Bad news from the brain: Descending 5-HT pathways that control pain processing. TRENDS in Pharmacological Sciences. 2004; 25(12). DOI:https://doi.org/10.1016/j.tips.2004.10.002
91. Gardner W.J. et al. Suppression of Pain by Sound. Science 132 (3418), 32-33. DOI:https://doi.org/10.1126/science.132.3418.32
92. Robson J.G. and Davenport H.T. The Effects of White Sound and Music upon the Superficial Pain Threshold. Canadian Anaesthetists’ Society journal.1962;9:105-8. DOI:https://doi.org/10.1007/BF03021250
93. Fink D.J. What is a Safe Noise Level for the Public. American Journal of Public Health. 2017; 107(1): 44-45. DOI:https://doi.org/10.2105/AJPH.2016.303527